Publications

Mechanical properties of extrinsic foot muscles, Achilles tendon, and plantar fascia in patients with a history of diabetic foot ulcers
Authors: Fatmagül Varol 1, Ali Ilez 2, Yavuz Aslan 3
Affiliations:
- Gulhane Faculty of Physiotherapy and Rehabilitation, Orthopedic Physiotherapy and Rehabilitation Department, University of Health Sciences, Emrah, Gata, Kecioren/Ankara 06010, Turkey
- Faculty of Health Science, Department of Physiotherapy and Rehabilitation, Istanbul Beykent University, Istanbul, Turkey
- Department of Underwater and Hyperbaric Medicine, University of Health Sciences, Sultan 2nd Abdulhamid Han Training and Research Hospital, Istanbul, Turkey
Journal: BMC Musculoskeletal Disorders - May 2025, Volume 26, Article no. 531 (DOI: 10.1186/s12891-025-08791-w)
-
Field & Applications:
- Medical
- Endocrinology
- Diabetes
- Validity
- Evaluating tissue mechanical properties using a simple and non-invasive technique, such as myotonometry, may serve as a practical tool for the early detection of diabetes-associated foot complications.
- Incorporating routine biomechanical assessments into diabetic foot care may allow for the early identification of at-risk individuals and facilitate timely, personalized preventive strategies.
Background: Diabetic foot ulcers (DFU) are a major complication of diabetes, often leading to impaired mobility and increased risk of recurrence due to persistent biomechanical alterations. Understanding the mechanical properties of foot muscles, tendons, and fascia may provide insight into ulcer development, prevention and rehabilitation strategies. This study aimed to assess the biomechanical properties of the extrinsic foot muscles, Achilles tendon (AT), and plantar fascia (PF) in individuals with a history of DFU using myotonometry.
Methods: A total of 38 diabetic feet with a history of DFU (Wagner Grade 0–1) and 40 healthy controls (HC) were evaluated. The MyotonPRO device was used to measure muscle tone (Natural Oscillation Frequency, F), stiffness, and elasticity in the tibialis anterior (TA), gastrocnemius medialis (GM), gastrocnemius lateralis (GL), AT, and PF. Measurements were performed in standardized positions, with statistical comparisons made between groups using independent t-tests.
Results: TA and GM showed significantly increased muscle tone and stiffness in the DFU group compared to HC (p < 0.05), whereas GL did not exhibit significant differences. Similarly, PF and AT stiffness were higher in the DFU group (p < 0.05), suggesting alterations in tissue load distribution. No significant differences in elasticity were observed between groups.
Conclusions: This study highlights persistent mechanical alterations in the TA, GM, AT, and PF in individuals with a history of DFU, despite ulcer healing. The increased stiffness and tone in these structures may contribute to abnormal foot loading patterns, potentially increasing the risk of ulcer recurrence. The findings emphasize the importance of early biomechanical assessment and targeted rehabilitation strategies, such as neuromuscular training, load redistribution, Achilles tendon stretching and custom orthotic interventions to mitigate mechanical dysfunction in diabetic foot patients.
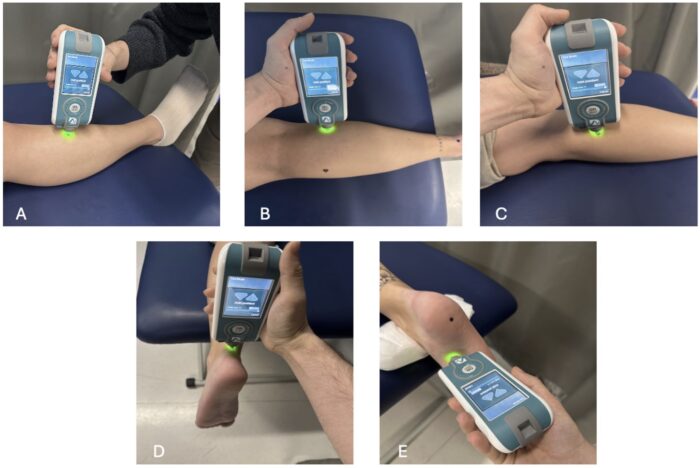
Figure 1. Myotonometric assessment of lower limb muscles and soft tissues. (A) Measurement over the tibialis anterior at the muscle belly in a supine position. (B) Assessment of the gastrocnemius lateralis at the muscle belly in a prone position. (C) Measurement over the gastrocnemius medialis at the muscle belly in a prone position. (D) Evaluation of the Achilles tendon at 4 cm above the calcaneal insertion in a neutral position. (E) Assessment of the plantar fascia at its proximal insertion near the calcaneus. Standardized measurement positions were maintained across all participants
Keywords: diabetic foot ulcer, tone, stiffness, extrinsic foot muscles, MyotonPRO
In conclusion, increased plantar fascia (PF) stiffness, along with elevated Achilles tendon (AT) stiffness and higher gastrocnemius medialis (GM) tone, was observed in individuals with diabetes and a history of previous foot ulcers. These findings indicate that mechanical alterations in foot structures persist even after ulcer healing, potentially leading to long-term biomechanical dysfunction and an increased risk of recurrence.
Considering the early involvement of intrinsic foot muscles in diabetes, progressive soft tissue stiffening may be a key factor contributing to ulcer recurrence. Addressing these mechanical changes through targeted rehabilitation strategies could help mitigate the risk of future complications. Stretching programs may enhance soft tissue flexibility, neuromuscular training could improve muscle function and coordination, and orthotic interventions may assist in redistributing plantar pressure to optimize foot mechanics.
Incorporating routine biomechanical assessments into diabetic foot care may allow for the early identification of at-risk individuals and facilitate timely, personalized preventive strategies. Determination of tissue mechanical properties with a simple method such as a myotonometer may be useful in the early diagnosis of diabetes-associated foot ulceration. Integrating the assessment of key tissue mechanical parameters – such as muscle tone, stiffness, and elasticity – into routine diabetic foot evaluations may enhance preventive strategies and improve long-term clinical outcomes.
By identifying and addressing underlying mechanical dysfunctions, these measures have the potential to reduce ulcer recurrence, improve mobility, and enhance the quality of life in individuals with diabetes. Incorporating such parameters into standard screening protocols could also help reduce the healthcare burden associated with ulcer treatment and lower-extremity amputations.


